Hearing the words “You have type 2 diabetes” can be a shock. It's a moment that can leave you feeling overwhelmed and uncertain about the future. You might be wondering how this diagnosis will change your life, what it means for your health, and if you'll ever be able to enjoy your favorite foods again. But take heart. This isn't the end of the road; it's simply a new path to navigate. And with the right information and support, you can not only live with diabetes but truly thrive. This guide is designed to be your companion on this journey, providing you with the knowledge and tools you need to take control of your health and live a full and vibrant life.

Understanding the Landscape: What is Type 2 Diabetes?
Your Body's Energy System
To understand type 2 diabetes, it helps to picture your body as a complex network, with glucose (sugar) serving as its primary fuel source. Think of glucose as the energy that keeps everything running smoothly. Now, imagine insulin, a hormone produced by your pancreas, as the key that unlocks your cells, allowing glucose to enter and provide energy.
In type 2 diabetes, this system encounters a problem. Either your body doesn't produce enough insulin, or your cells become resistant to it, like a lock that's become stiff and difficult to open. This is known as insulin resistance. When this happens, glucose can't get into your cells effectively, leading to a buildup of sugar in your bloodstream. Over time, this excess blood sugar can damage your blood vessels and nerves, increasing your risk of serious health complications.
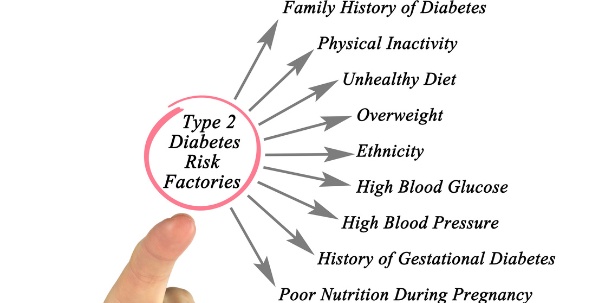
Unraveling the Risk Factors: Why Me?
Several factors can increase your likelihood of developing type 2 diabetes. Some of these, like your family history and genetic predisposition, are beyond your control. However, other factors are within your power to influence. These modifiable risk factors include:
- Weight: Being overweight or obese significantly increases your risk.
- Physical Inactivity: A sedentary lifestyle contributes to insulin resistance.
- Unhealthy Diet: A diet high in processed foods, sugary drinks, and unhealthy fats can increase your risk.
- Age: Your risk increases as you get older, especially after age 45.
- Family History: Having a parent or sibling with type 2 diabetes increases your risk.
- Ethnicity: Certain ethnic groups, such as African Americans, Hispanic Americans, Native Americans, and Asian Americans, have a higher risk.
Understanding these risk factors is not about blaming yourself but about empowering you to make informed choices that can positively impact your health.
Charting Your Course: Managing Type 2 Diabetes
Managing type 2 diabetes is a multifaceted journey that involves several key strategies working together. Think of it as a tripod, with each leg playing a crucial role in supporting your overall well-being.
1. Nourishing Your Body: The Power of Diet

What you eat has a direct impact on your blood sugar levels. This doesn't mean you have to give up all your favorite foods, but it does mean making conscious choices about what you fuel your body with. A diabetes-friendly diet focuses on:
- Choosing whole, unprocessed foods: These include fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Limiting processed foods, sugary drinks, and unhealthy fats: These can spike your blood sugar levels and contribute to weight gain.
- Monitoring carbohydrate intake: Carbohydrates are broken down into glucose, so it's important to be mindful of your portion sizes and choose complex carbohydrates over simple ones.
- Spreading your carbohydrate intake throughout the day: This helps to prevent blood sugar spikes.
A Week of Diabetes-Friendly Meals
To help you get started, here's a sample 7-day meal plan that incorporates delicious and nutritious options while keeping carbohydrate intake in check:
Day 1
- Breakfast (264 cal, 18g carbs): Greek yogurt (1.5 cups, nonfat, plain), blackberries (1/2 cup), chopped walnuts (2 tablespoons).
- Morning Snack (170 cal, 21g carbs): 2 clementines, 10 almonds (about 1/2 ounce).
- Lunch (360 cal, 30g carbs):White Bean & Veggie Salad (1 serving).
- Afternoon Snack (114 cal, 14g carbs): Raspberries (1 cup), 1 string cheese (about 1 ounce).
- Dinner (550 cal, 30g carbs): Ginger-Tahini Oven-Baked Salmon & Vegetables (1 serving).
- Evening Snack (40 cal, 6g carbs): 1/2 cup cucumber slices with 1 tablespoon hummus.
Total: 1498 calories
Day 2
- Breakfast (288 cal, 22g carbs):Muffin-Tin Omelets with Feta & Peppers (1 serving), medium orange.
- Morning Snack (200 cal, 5g carbs): 1 small cucumber with 2 tablespoons almond butter.
- Lunch (360 cal, 10g carbs): Avocado Grilled Chicken Salad (1 serving).
- Afternoon Snack (75 cal, 15g carbs): Sliced large bell pepper, 1 medium carrot.
- Dinner (418 cal, 14g carbs):Homemade Chicken Tenders with Everything Bagel Seasoning over Salad (1 serving), 1/2 avocado.
- Evening Snack (160 cal, 6g carbs): 1 cup low-fat cottage cheese.
Total: 1501 calories
Day 3
- Breakfast (288 cal, 22g carbs):Muffin-Tin Omelets with Feta & Peppers (1 serving), medium orange.
- Morning Snack (148 cal, 19g carbs): 2 clementines, 1 boiled egg (large).
- Lunch (360 cal, 10g carbs): Avocado Grilled Chicken Salad (1 serving).
- Afternoon Snack (230 cal, 16g carbs): Greek yogurt (1.5 cups, nonfat, plain) with Berries (1/2 cup)
- Dinner (525 cal, 25g carbs):Chicken Cutlets with Sun-Dried Tomato Cream Sauce (1 serving), steamed broccoli florets (3 cups).
- Evening Snack (40 cal, 6g carbs): 1/2 cup cucumber slices with 1 tablespoon hummus.
Total: 1591 calories
Day 4
- Breakfast (277 cal, 30g carbs):Blueberry Almond Chia Pudding (1 servings).
- Morning Snack (52 cal, 4.5g carbs): 1/4 cup cottage cheese (low-fat) with 3 cucumber slices.
- Lunch (360 cal, 10g carbs): Avocado Grilled Chicken Salad (1 serving).
- Afternoon Snack (306 cal, 8g carbs): Muffin-Tin Omelets with Feta & Peppers (1 serving), 1 string cheese (about 1 ounce).
- Dinner (376 cal, 21g carbs):Sheet-Pan Maple-Mustard Pork Chops & Carrots (1 serving).
- Evening Snack (190 cal, 29g carbs): 1 medium apple, 1 tablespoon peanut butter.
Total: 1561 calories
Day 5
- Breakfast (277 cal, 30g carbs):Blueberry Almond Chia Pudding (1 servings).
- Morning Snack (135 cal, 6g carbs): Nonfat plain Greek yogurt (1 cup).
- Lunch (360 cal, 10g carbs): Avocado Grilled Chicken Salad (1 serving).
- Afternoon Snack (160 cal, 6g carbs): Dry-roasted unsalted almonds (20 pieces, about 1 ounce).
- Dinner (490 cal, 27g carbs):No-Noodle Eggplant Lasagna (1 serving), Traditional Greek Salad (1 serving).
- Evening Snack (90 cal, 15g carbs): 1/2 cup mango slices with 1/4 cup non-fat Greek yogurt.
Total: 1512 calories
Day 6
- Breakfast (322 cal, 19g carbs): Greek yogurt (1.5 cups, nonfat, plain), blackberries (1/2 cup), chopped walnuts (2 tablespoons).
- Morning Snack (130 cal, 17g carbs): 1 small apple with 10 almonds
- Lunch (348 cal, 30g carbs):No-Noodle Eggplant Lasagna (1 serving), pomegranate seeds (1/3 cup).
- Afternoon Snack (92 cal, 6g carbs): 1/2 cup low-fat cottage cheese with 3 cucumber slices
- Dinner (428 cal, 17g carbs):Tofu & Vegetable Curry with Zucchini Noodles (1 serving).
- Evening Snack (97 cal, 9g carbs): 10-12 almonds with 1/2 cup strawberries.
Total: 1417 calories
Day 7
- Breakfast (288 cal, 22g carbs):Muffin-Tin Omelets with Feta & Peppers (1 serving), medium orange.
- Morning Snack (170 cal, 25g carbs): Medium carrots, sliced (4), 1 boiled egg (large).
- Lunch (337 cal, 26g carbs):No-Noodle Eggplant Lasagna (1 serving), sliced medium bell pepper.
- Afternoon Snack (85 cal, 6.5g carbs): Greek yogurt (1/2 cups, nonfat, plain) with Berries (1/4 cup)
- Dinner (519 cal, 13g carbs):Shrimp Cauliflower Fried Rice (1 serving), mixed greens (2 cups), Homemade Vinaigrette with Sesame & Ginger (1 serving), 1/2 avocado.
- Evening Snack (120 cal, 24g carbs): Frozen yogurt (1/2 cup).
Total: 1519 calories
This meal plan is a starting point, and you can adapt it to your preferences and dietary needs. It's always a good idea to consult with a registered dietitian or a certified diabetes educator. They can help you create a personalized meal plan that aligns with your individual goals and health conditions.
2. Moving Your Body: The Benefits of Exercise

Physical activity is a powerful tool in managing type 2 diabetes. When you engage in regular exercise, your muscles become more sensitive to insulin, allowing them to use glucose more effectively. This helps to lower your blood sugar levels and reduce your risk of diabetes-related complications.
Finding Your Fitness Rhythm
The most effective exercise is the one you enjoy and can stick with in the long run. It doesn't have to involve intense gym workouts. Find activities that fit your lifestyle and preferences, whether it's brisk walking, swimming, dancing, cycling, or even gardening. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
Here are some ideas to get you moving:
- Walking: Start with short walks and gradually increase the duration and intensity. Explore your neighborhood, walk with a friend, or join a walking group.
- Swimming: This is a great low-impact option that's gentle on your joints.
- Yoga: Yoga combines physical postures with breathing exercises and meditation, which can help to reduce stress and improve flexibility.
- Dancing: Put on some music and move to the beat! Dancing is a fun way to get your heart rate up and improve your mood.
Remember to start slowly and gradually increase the intensity and duration of your activities. It's also important to listen to your body and take rest days when needed.
3. Medication: A Helping Hand

While lifestyle changes are essential, sometimes they may not be enough to manage blood sugar levels effectively. In these cases, your doctor may prescribe medication to help your body produce or use insulin more effectively.
Understanding Your Options
There are several types of diabetes medications available, each working in a different way:
- Metformin: This is often the first medication prescribed for type 2 diabetes. It works by decreasing the amount of glucose produced by your liver and improving your body's sensitivity to insulin.
- Sulfonylureas: These medications stimulate your pancreas to release more insulin.
- DPP-4 Inhibitors: These help your body produce more insulin after meals by preventing the breakdown of a natural incretin hormone that promotes insulin release.
- SGLT2 Inhibitors: These work by blocking the reabsorption of glucose in your kidneys, allowing excess glucose to be excreted in your urine.
- GLP-1 Receptor Agonists: These medications mimic the effects of a natural incretin hormone, stimulating insulin release and reducing glucagon secretion (a hormone that raises blood sugar).
Your doctor will work with you to determine the most appropriate medication and dosage based on your individual needs and health history.
4. Monitoring Your Blood Sugar: Staying Informed

Regularly monitoring your blood sugar levels is crucial for tracking your progress and making any necessary adjustments to your treatment plan. Your doctor will advise you on how often to check your blood sugar and what your target range should be.
Methods for Monitoring
Fingerstick Glucose Meter: This is the most common method. It involves pricking your finger with a small lancet to obtain a blood sample, which is then applied to a test strip inserted into the meter. The meter then displays your blood sugar level.
Continuous Glucose Monitor (CGM): This is a small, wearable device that continuously monitors your glucose levels throughout the day and night. It consists of a sensor inserted under your skin, usually on your abdomen or arm, that measures glucose levels in the fluid surrounding your cells. This information is then wirelessly transmitted to a receiver, which can be a separate device or integrated into a smartphone or insulin pump. CGMs provide a more dynamic picture of your blood sugar fluctuations, showing trends and patterns that you might miss with traditional fingerstick testing. This can be particularly helpful in identifying high or low blood sugar levels early on, allowing you to take action to prevent potential problems.
5. Stress Management: Finding Your Calm

Stress can have a significant impact on your blood sugar levels. When you're stressed, your body releases hormones like cortisol and adrenaline, which can raise your blood sugar. Finding healthy ways to manage stress is an essential part of your diabetes management plan.
Techniques for Stress Reduction
Mindfulness Meditation: This involves focusing on the present moment without judgment. Even a few minutes of daily meditation can help to reduce stress and improve your overall well-being. There are many guided meditation apps and resources available to help you get started.
Deep Breathing Exercises: Deep, slow breaths can help to activate your body's relaxation response. Try practicing diaphragmatic breathing, where you inhale deeply into your abdomen, allowing your belly to rise, and exhale slowly.
Progressive Muscle Relaxation: This technique involves systematically tensing and relaxing different muscle groups in your body. It can help to release physical tension and promote relaxation.
Yoga and Tai Chi: These practices combine physical postures with breathing exercises and mindfulness, promoting relaxation and reducing stress.
Spending Time in Nature: Studies have shown that spending time outdoors can lower stress hormone levels and improve mood. Take a walk in the park, go for a hike, or simply sit and enjoy the scenery.
Engaging in Hobbies: Make time for activities you enjoy, whether it's reading, painting, gardening, or listening to music. Hobbies can provide a sense of relaxation and help you to de-stress.
Connecting with Loved Ones: Social support is crucial for managing stress. Spend time with friends and family, talk to a trusted confidante, or join a support group.
6. Sleep: The Restorative Power

Getting enough quality sleep is vital for your overall health and well-being, and it plays a particularly important role in managing type 2 diabetes. When you don't get enough sleep, your body becomes less sensitive to insulin, which can lead to higher blood sugar levels.
Tips for a Restful Night's Sleep
Establish a Consistent Sleep Schedule: Go to bed and wake up around the same time each day, even on weekends, to regulate your body's natural sleep-wake cycle.
Create a Relaxing Bedtime Routine: Wind down in the hour or two before bed by taking a warm bath, reading a book, listening to calming music, or practicing relaxation techniques.
Optimize Your Sleep Environment: Make sure your bedroom is dark, quiet, and cool. Consider using blackout curtains, earplugs, or a white noise machine to block out distractions.
Limit Screen Time Before Bed: The blue light emitted from electronic devices can interfere with your sleep. Avoid using screens for at least an hour before bedtime.
Watch Your Diet: Avoid caffeine and alcohol in the hours leading up to sleep, as they can disrupt your sleep patterns.
Get Regular Exercise: Physical activity can improve sleep quality, but avoid exercising too close to bedtime.
Thriving with Diabetes: Embracing Your Journey

A diagnosis of type 2 diabetes may require adjustments, but it doesn't have to define you. With the right approach, you can live a full, active, and rewarding life.
Building a Support Network
You are not alone on this journey. Connecting with others who understand what you're going through can provide invaluable support and encouragement. Consider joining a diabetes support group, either in person or online, where you can share experiences, learn from others, and find a sense of community. Talking to a therapist or counselor can also provide emotional support and help you develop coping strategies.
Becoming an Informed Advocate for Your Health
Knowledge is empowering. The more you understand about diabetes, the better equipped you'll be to manage it effectively. Read books, articles, and reliable online resources from reputable organizations like the American Diabetes Association (ADA) or the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Attend diabetes education classes or workshops to learn more about self-care strategies. Don't hesitate to ask your doctor questions and actively participate in your treatment plan.
Setting Achievable Goals
Making significant lifestyle changes can feel daunting. Instead of trying to overhaul everything at once, start by setting small, achievable goals. Perhaps you want to start by walking for 15 minutes a day, incorporating more vegetables into your meals, or trying a new stress-reduction technique. As you achieve these smaller goals, you'll build confidence and motivation to tackle larger ones.
Prioritizing Self-Care
Managing diabetes requires ongoing effort, and it's essential to prioritize self-care to avoid burnout. Make time for activities that help you relax, recharge, and nurture your well-being. This could include spending time in nature, listening to music, getting a massage, pursuing a hobby, or simply taking some quiet time for yourself.
Cultivating a Positive Mindset
A positive attitude can make a world of difference in how you cope with diabetes. Focus on the things you can control, celebrate your successes, and don't let diabetes define you. Remember that you are not alone, and millions of people are living full and meaningful lives with diabetes.
This journey with type 2 diabetes may have its challenges, but it's also an opportunity for self-discovery, resilience, and empowerment. By embracing a proactive approach to managing your health, you can navigate this new path with confidence and live a fulfilling life. Remember, this is your journey, and you have the power to shape it.
References
- Dietary Patterns and Incidence of Type 2 Diabetes in Older Women
- Effect of a Mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: a randomized trial
- Primary Prevention of Cardiovascular Disease with a Mediterranean Diet
- Exercise and Type 2 Diabetes: The American College of Sports Medicine and the American Diabetes Association: joint position statement
- Effect of aerobic and resistance training on hemoglobin A1c levels in patients with type 2 diabetes: a randomized controlled trial
- Metformin and Cardiovascular Disease in Type 2 Diabetes
- Efficacy and Safety of Once-Weekly Semaglutide Versus Once-Daily Sitagliptin as an Add-on to Metformin, With or Without Sulfonylurea, in Patients With Type 2 Diabetes (SUSTAIN 1): A Randomised, Open-label, Parallel-group, Multicentre, Phase 3a Trial
- Effectiveness of Continuous Glucose Monitoring on Glycemic Control in Patients With Type 2 Diabetes Mellitus: A Systematic Review and Meta-analysis
- Impact of mindfulness-based stress reduction (MBSR) on sleep, mood, stress and eating behaviors in adults with overweight or obesity
- Stress Reduction and Mindfulness-Based Interventions for Patients With Diabetes
- Sleep Duration as a Risk Factor for Diabetes Incidence in a Large US Sample
- The Association of Sleep Disorders With Diabetes Mellitus: A Population-Based Study