Imagine a world where a tiny army of microscopic allies resides within your gut, tirelessly working to keep your blood sugar balanced and your energy levels stable. What if these allies could help prevent the debilitating complications of diabetes and even offer a glimmer of hope for reversing the condition altogether? This isn't science fiction – it's the fascinating world of probiotics and their potential to revolutionize how we approach diabetes.
The Gut Microbiome: Your Inner Ecosystem
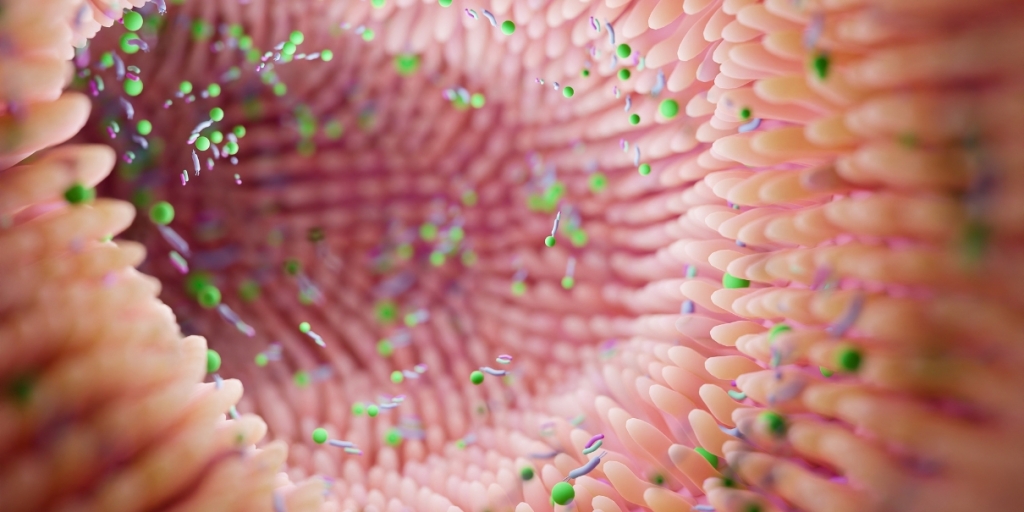
Before we delve into the power of probiotics, let's take a closer look at the bustling metropolis within your digestive system: the gut microbiome. This complex community of trillions of bacteria, fungi, viruses, and other microorganisms plays a far more significant role in your health than you might imagine.
Think of your gut microbiome as a rainforest teeming with diverse life. Just like a balanced ecosystem is crucial for a thriving rainforest, a balanced gut microbiome is essential for your overall well-being. These microscopic residents help digest your food, produce essential vitamins, and train your immune system. But perhaps most importantly, they influence your metabolism and how your body regulates blood sugar.
The Link Between Gut Health and Diabetes
Emerging research suggests that an imbalance in the gut microbiome, known as dysbiosis, may be a key player in the development of both type 1 and type 2 diabetes. In type 1 diabetes, an autoimmune attack destroys the insulin-producing cells in the pancreas. Studies have shown that individuals with type 1 diabetes often have a less diverse gut microbiome with lower levels of beneficial bacteria. For instance, a 2014 study in Diabetologia found that children with type 1 diabetes had lower levels of bacteria producing butyrate, a short-chain fatty acid that plays a role in gut health and immune regulation.
In type 2 diabetes, the body becomes resistant to insulin, the hormone that allows glucose to enter cells for energy. Dysbiosis can contribute to insulin resistance by triggering inflammation and disrupting the signaling pathways that regulate blood sugar. A 2013 study in Nature showed that people with type 2 diabetes had altered gut microbiota compared to healthy individuals, with an increase in inflammation-promoting bacteria.
Probiotics: The Tiny Allies in Your Gut
This is where probiotics enter the picture. Probiotics are live microorganisms that, when consumed in adequate amounts, confer health benefits to the host. You can find them in fermented foods like yogurt, kefir, sauerkraut, and kimchi, or in supplement form.
Think of probiotics as reinforcements for your gut's microscopic army. They help restore balance to the microbiome, increasing the number of beneficial bacteria and crowding out harmful ones. But how exactly can these tiny allies help manage and potentially even reverse diabetes?
Mechanisms of Action
Probiotics exert their influence on diabetes through a variety of mechanisms:
-
Improved Insulin Sensitivity: Certain probiotic strains, such as Bifidobacterium infantis and Lactobacillus acidophilus, have been shown to enhance insulin sensitivity. They do this by influencing the composition of the gut microbiota and increasing the production of short-chain fatty acids like butyrate, which have been shown to improve insulin signaling. Imagine these probiotics as tiny messengers that help your cells communicate better with insulin, allowing glucose to enter the cells more effectively.
-
Reduced Inflammation: Chronic inflammation is a hallmark of diabetes and contributes to its progression. Probiotics can help dampen inflammation in the gut and throughout the body, potentially slowing the disease's course. For example, Lactobacillus reuteri has been shown to reduce inflammation by modulating the immune response and decreasing the production of pro-inflammatory cytokines.
-
Increased Incretin Production: Incretins are hormones that stimulate insulin release and suppress glucagon secretion, another hormone that raises blood sugar levels. Some probiotics, like Bifidobacterium bifidum, have been found to increase incretin production, further aiding in blood sugar regulation. They achieve this by influencing the gut microbiota and promoting the release of GLP-1, a key incretin hormone.
-
Strengthened Gut Barrier: A “leaky gut” allows harmful substances to pass into the bloodstream, triggering inflammation and potentially contributing to insulin resistance. Probiotics can help strengthen the gut barrier, preventing this leakage and its associated problems. Think of them as reinforcing the walls of your gut, keeping harmful substances out and beneficial ones in.
Research and Evidence: A Closer Look at Specific Strains
While research on probiotics and diabetes is still ongoing, numerous studies have shown promising results. Here's a closer look at some specific strains and their potential benefits:
-
Type 1 Diabetes: A 2015 study published in the journal Diabetes/Metabolism Research and Reviews found that supplementing with a multi-strain probiotic containing Lactobacillus acidophilus, Lactobacillus casei, Bifidobacterium bifidum, and Lactobacillus rhamnosus in children with type 1 diabetes led to improved blood sugar control and reduced insulin requirements. These strains may help modulate the immune response and protect against the destruction of insulin-producing cells.
-
Type 2 Diabetes: A 2016 meta-analysis of 12 randomized controlled trials published in the journal Clinical Nutrition concluded that probiotic supplementation, particularly with strains like Lactobacillus acidophilus, Lactobacillus casei, and Bifidobacterium lactis, significantly reduced fasting blood glucose and HbA1c (a measure of long-term blood sugar control) in individuals with type 2 diabetes.
It's important to note that the effectiveness of probiotics can vary depending on the individual, the specific strains used, and the dosage. More research is needed to determine the optimal strains and dosages for different types of diabetes.
Dosage and Safety Considerations
When it comes to probiotic supplementation, dosage matters. While general recommendations can be helpful, it's essential to consult with your doctor to determine the appropriate dosage for your individual needs.
-
General Guidelines: For diabetes management, studies have typically used dosages ranging from 10 billion to 100 billion colony-forming units (CFUs) per day. It's often recommended to start with a lower dosage and gradually increase it as needed.
-
Safety: Probiotics are generally safe for most people. However, some individuals may experience mild side effects like gas or bloating, especially when first starting a probiotic supplement. In rare cases, people with compromised immune systems may experience more serious side effects. Always talk to your doctor before starting any new supplement, especially if you have any underlying health conditions or are taking medications.
Addressing Limitations and Counterpoints
While the research on probiotics and diabetes is promising, it's important to acknowledge some limitations.
-
Variability in Study Designs: Studies on probiotics and diabetes have used different strains, dosages, and durations of treatment, making it difficult to draw definitive conclusions.
-
Need for Long-Term Studies: More long-term studies are needed to assess the sustained effects of probiotics on diabetes management and the prevention of complications.
-
Conflicting Studies: While many studies have shown positive results, some studies have not found significant benefits of probiotics in diabetes management. This highlights the need for further research to understand the complex interactions between probiotics, the gut microbiome, and diabetes.
Beyond Blood Sugar: Probiotics and Diabetes Complications

The benefits of probiotics extend beyond just blood sugar control. Diabetes can lead to a range of complications affecting various organs, and probiotics may offer protection against some of these:
Kidney Health
Diabetic nephropathy, or kidney disease, is a serious complication of diabetes. High blood sugar levels damage the kidneys' delicate filtering system, leading to protein in the urine, swelling, and eventually kidney failure. Studies suggest that probiotics may help protect kidney function in people with diabetes. For example, a 2019 study published in the journal “PLOS One” found that a probiotic supplement containing Lactobacillus acidophilus and Bifidobacterium lactis reduced markers of kidney damage in patients with type 2 diabetes. These probiotics may help by reducing inflammation and oxidative stress in the kidneys.
Nerve Health
Diabetic neuropathy, or nerve damage, is another common complication. High blood sugar can injure nerves throughout the body, causing numbness, tingling, pain, and even loss of sensation. Probiotics may help protect against nerve damage by reducing inflammation and oxidative stress. A 2015 study in the journal “Diabetes & Metabolism” showed that probiotic supplementation with Lactobacillus acidophilus improved nerve function and reduced pain in patients with diabetic neuropathy.
Heart Health
People with diabetes are at increased risk for cardiovascular disease. Probiotics may help improve heart health by lowering cholesterol levels, reducing blood pressure, and improving blood vessel function. A 2019 review article in the journal “Nutrients” summarized several studies demonstrating the positive effects of probiotics, including Lactobacillus plantarum and Bifidobacterium longum, on cardiovascular risk factors in people with diabetes.
The Future of Probiotics in Diabetes Management
The research on probiotics and diabetes is rapidly evolving, and the future holds exciting possibilities. Scientists are working to identify specific probiotic strains that are most effective for different types of diabetes and its complications. They are also exploring the use of probiotics in combination with prebiotics (non-digestible food ingredients that promote the growth of beneficial bacteria) to further enhance their effectiveness. Imagine a future where your doctor can prescribe a personalized probiotic blend, like a tailored medication, to address your specific needs.
Personalized Probiotic Therapy
One promising area of research is personalized probiotic therapy. Just as our genes and lifestyles differ, so do our gut microbiomes. In the future, healthcare providers may be able to analyze an individual's gut microbiome and recommend specific probiotic strains tailored to their needs. This personalized approach could revolutionize diabetes management and lead to more targeted and effective treatments. However, implementing personalized probiotic therapies in clinical practice faces challenges, such as the need for standardized methods for microbiome analysis and the development of individualized probiotic formulations.
Probiotics as a Preventative Measure
Could probiotics help prevent diabetes in the first place? Some studies suggest that early intervention with probiotics may help modulate the gut microbiome and reduce the risk of developing diabetes. For example, a 2017 study in the journal Diabetes Care found that supplementing with Lactobacillus rhamnosus GG during pregnancy and early infancy reduced the risk of type 1 diabetes in children with a genetic predisposition. This is an area of active research, and future studies may provide more definitive answers.
Practical Tips for Incorporating Probiotics
If you're interested in experiencing the benefits of probiotics, consider these practical tips for incorporating them into your daily routine:
Embrace Probiotic-Rich Foods: Many delicious foods naturally contain probiotics. Enjoy a daily serving of yogurt with “live and active cultures,” explore the tangy flavor of kefir, or add sauerkraut and kimchi to your meals for a flavorful probiotic boost. Tempeh and miso are also excellent sources of probiotics and can be incorporated into a variety of dishes.
Choose Supplements Wisely: If you prefer supplements, select those listing specific strains and their CFU count. Prioritize reputable brands that undergo third-party testing to ensure quality and potency. Always follow storage instructions carefully, as probiotics are living organisms that can be affected by heat and moisture.
Consult Your Healthcare Provider: Before starting any new supplement, especially if you have underlying health conditions or are taking medications, it's always wise to consult your doctor. They can provide personalized advice based on your individual needs and health status.
Be Patient and Consistent: Remember that it may take time to fully experience the benefits of probiotics. Be patient and consistent with your intake, whether through food or supplements, and allow your gut microbiome time to adjust and flourish.
A Personal Touch: My Journey with Probiotics
I've always been fascinated by the intricate workings of the human body, and the gut microbiome is no exception. When I was diagnosed with prediabetes a few years ago, I became even more interested in the connection between gut health and metabolic disease. I started incorporating probiotic-rich foods into my diet, like adding a daily serving of Greek yogurt with berries and a side of sauerkraut to my lunch. I also started taking a probiotic supplement containing Lactobacillus acidophilus and Bifidobacterium lactis. I noticed a significant improvement in my digestion and energy levels. While I can't attribute all the credit to probiotics, I believe they played a role in helping me reverse my prediabetes and maintain healthy blood sugar levels.
A Holistic Approach to Diabetes Management
Probiotics offer a promising new frontier in diabetes management. While they are not a cure-all, they represent a powerful tool that can work synergistically with other lifestyle interventions to improve blood sugar control, reduce the risk of complications, and enhance overall health.
As research continues to unravel the complex interplay between the gut microbiome and diabetes, we can expect to see even more innovative applications of probiotics in the years to come. By embracing a holistic approach that includes a healthy diet, regular exercise, medication as needed, and the power of probiotics, we can take charge of our health and live fulfilling lives with diabetes.