Imagine a world where the food you eat doesn't just nourish you but also actively fights against diabetes. It's not a fantasy, it's a reality within your reach. The right foods can not only help you manage your blood sugar but also potentially reverse the course of type 2 diabetes. So, let's ditch the fear and embark on a culinary adventure filled with flavor and health benefits.
What is Diabetes, Anyway?
Diabetes, often referred to as diabetes mellitus, isn't just about high blood sugar. It's a chronic metabolic disorder that throws a wrench in how your body uses glucose, the primary source of energy for your cells. Imagine glucose as the fuel that keeps your body's engine running smoothly. In diabetes, this fuel either can't get into the cells efficiently or isn't being utilized properly, leading to a buildup of glucose in your bloodstream.
The Role of Insulin
Normally, your pancreas produces a hormone called insulin. Think of insulin as the key that unlocks the doors of your cells, allowing glucose to enter and be used for energy. However, in people with diabetes, this key either isn't working properly or there aren't enough keys to go around.
The Different Types of Diabetes
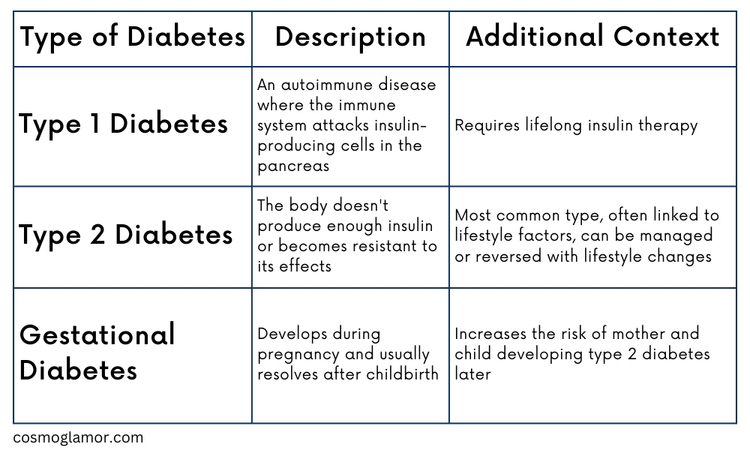
Diabetes is a complex condition, but understanding the basics is crucial for managing it effectively. By learning about the different types and causes of diabetes, you can take proactive steps to protect your health and live a fulfilling life. Whether you're newly diagnosed, prediabetic, or simply want to learn more, knowledge is your most powerful tool.
Prediabetes: The Silent Alarm
Prediabetes is like a whisper from your body, hinting that your blood sugar is too high—not yet diabetes, but a warning sign. Often, there are no symptoms, so it's easy to miss. But ignoring it can lead to type 2 diabetes and serious health problems. The good news? Prediabetes is reversible! Healthy eating, exercise, and even small weight loss can make a big difference. Think of it as a chance to hit the reset button on your health. Talk to your doctor about a plan to lower your blood sugar and avoid future complications.
Understanding the Glycemic Index: Your Blood Sugar's Best Friend
Imagine the glycemic index (GI) as a helpful speedometer for your blood sugar. It ranks carbohydrate-containing foods on a scale of 0 to 100, showing you how quickly they raise your blood glucose levels after you eat them. The higher the GI, the faster and higher your blood sugar spikes.
Why it Matters for Diabetes
For people with diabetes or prediabetes, keeping blood sugar levels stable is key. That’s where the GI comes in handy. By choosing foods with a low GI, you can help prevent those dramatic spikes and crashes that can leave you feeling tired, irritable, and hungry again soon after eating.
Low GI vs. High GI: What's the Difference?
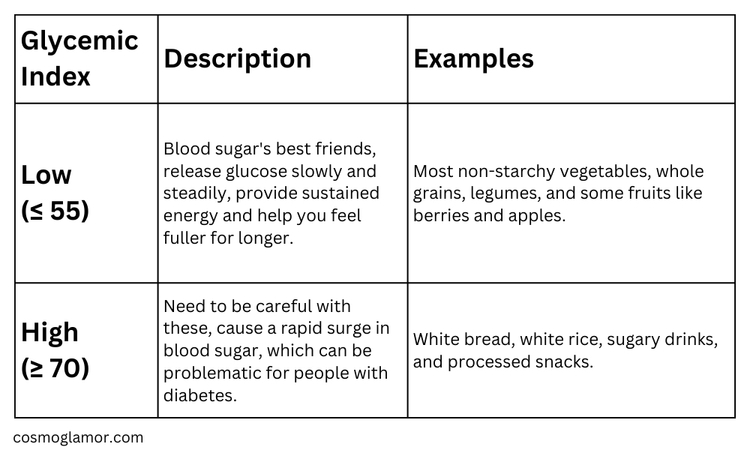
The GI is Not the Whole Story
While the GI is a valuable tool, it's important to remember that it's just one piece of the puzzle. The amount of carbohydrates you eat also plays a big role in how your blood sugar responds. That's why portion control is still essential, even when choosing low GI foods.
Making the GI Work for You
- Focus on Low GI Foods: Make them the foundation of your diet.
- Limit High GI Foods: Enjoy them occasionally and in moderation.
- Read Food Labels: Pay attention to the carbohydrate content and GI of packaged foods.
- Combine Foods Wisely: Pair high GI foods with protein and healthy fats to slow down their absorption.
Remember, managing your blood sugar doesn't have to be a guessing game. By understanding the glycemic index and making informed food choices, you can take control of your diabetes and live a healthier, happier life.
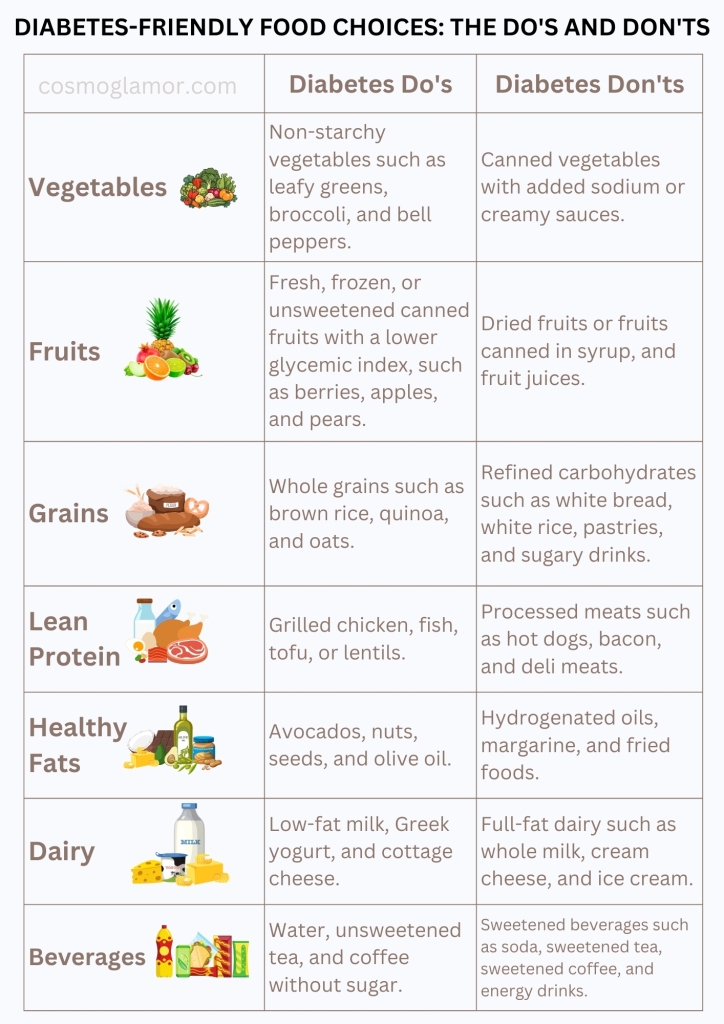
The Do's and Don'ts of Diabetic Dining
Think of your plate as a canvas for vibrant health, where every food choice paints a picture of balanced blood sugar and long-term well-being. Let's break down the key players in this culinary masterpiece – the foods that deserve a starring role and those that are better left off the stage.
Diabetes Do's: The Nutritional All-Stars
-
Vegetables: These are the unsung heroes of any healthy diet, and for people with diabetes, they're especially important. Packed with fiber, vitamins, and minerals, non-starchy vegetables like leafy greens, broccoli, and bell peppers are low in carbs and help keep blood sugar levels steady. They also add bulk to your meals, keeping you feeling full and satisfied.
-
Fruits: While fruits contain natural sugars, they can still be part of a diabetes-friendly diet when enjoyed in moderation. Opt for fresh, frozen, or unsweetened canned fruits with a lower glycemic index, such as berries, apples, and pears.
-
Whole Grains: Unlike their refined counterparts, whole grains like brown rice, quinoa, and oats are rich in fiber, which slows down the absorption of glucose into your bloodstream. This helps prevent blood sugar spikes and keeps you feeling energized for longer.
-
Lean Protein: Whether it's grilled chicken, fish, tofu, or lentils, protein is essential for building and repairing tissues. It also helps stabilize blood sugar levels and promotes satiety. Choose lean cuts of meat and poultry, and try to include plant-based protein sources like beans and legumes regularly.
-
Healthy Fats: Avocados, nuts, seeds, and olive oil provide heart-healthy fats that can improve insulin sensitivity and reduce the risk of heart disease, a major concern for people with diabetes. Plus, they add flavor and richness to your meals, making healthy eating even more enjoyable.
Diabetes Don'ts: The Unwanted Guests
-
Refined Carbohydrates: These include white bread, white rice, pastries, and sugary drinks. They're quickly digested, leading to rapid blood sugar spikes and crashes. They also offer little nutritional value, so it's best to limit them as much as possible.
-
Processed Meats: Hot dogs, bacon, and deli meats are high in saturated fat and sodium, which can increase your risk of heart disease and high blood pressure. Opt for lean protein sources instead.
-
Sugary Drinks: Sodas, fruit juices, and energy drinks are loaded with added sugars, which can wreak havoc on your blood sugar levels. Stick to water, unsweetened tea, or coffee for hydration.
-
Fried Foods: These are high in unhealthy fats and calories, which can contribute to weight gain and worsen insulin resistance. Choose baked, grilled, or steamed options instead.
The Meal Plate: Your Visual Guide to Portion Control
When it comes to managing diabetes, portion control isn’t just helpful – it's essential. Think of your plate as a visual guide to building a balanced meal. The plate method offers a simple, yet effective way to ensure you're getting the right amount of each food group without needing to measure or weigh everything.
How it Works
Imagine your plate divided into sections:
- Half your plate: Pile this section high with non-starchy vegetables. Think vibrant colors and a variety of textures – leafy greens, broccoli florets, sliced bell peppers, or roasted asparagus.
- Quarter of your plate: This section is reserved for lean protein. Grilled chicken breast, baked salmon, a scoop of lentils, or a handful of tofu cubes would fit perfectly here.
- Quarter of your plate: Fill this last quarter with carbohydrate-rich foods like whole grains. A small serving of brown rice, quinoa, or a slice of whole-wheat bread are good options.
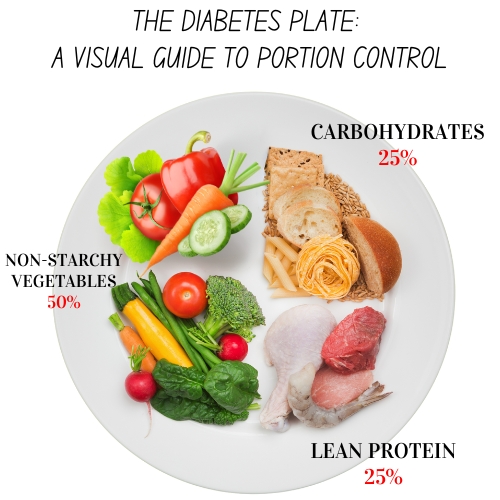
Beyond the Plate
The plate method is a great starting point, but don't forget to include:
- A serving of healthy fats: A drizzle of olive oil on your veggies, a few slices of avocado, or a sprinkle of nuts or seeds can add flavor and help you feel satisfied.
- A glass of water or unsweetened beverage: Stay hydrated and avoid sugary drinks that can spike your blood sugar.
Remember:
- Portion sizes can vary depending on your individual needs and activity level. It's always best to consult with a registered dietitian or healthcare professional to tailor the plate method to your specific goals.
- The plate method isn't just for dinner! You can use it for breakfast, lunch, and snacks too. Just adjust the portions accordingly.
The plate method is a simple yet powerful tool that takes the guesswork out of portion control. By visualizing your meals, you can make healthier choices, manage your blood sugar levels, and still enjoy a variety of delicious foods.
A Sample Meal Plan: Delicious and Diabetes-Friendly
To give you a taste of what a balanced diabetic meal plan can look like, let's explore a sample day of eating that's both nutritious and enjoyable. Remember, this is just an example, and it's always recommended to personalize your plan with the help of a healthcare professional.
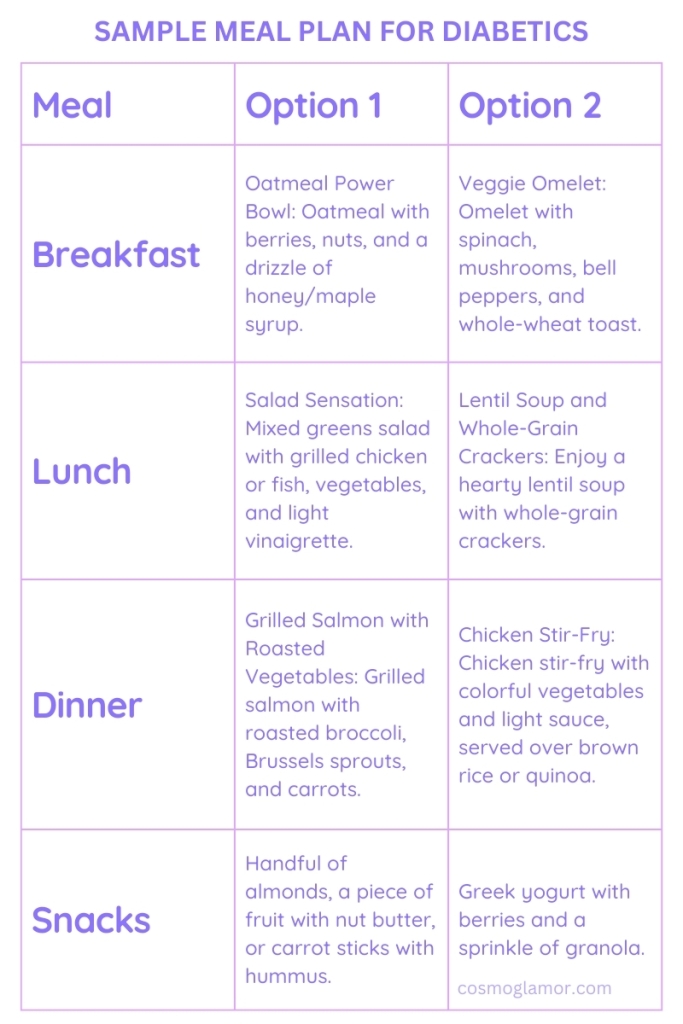
Key Points:
- Variety is key: Don't be afraid to mix and match different foods and flavors to keep your meals exciting.
- Prioritize whole foods: Choose whole, unprocessed foods whenever possible.
- Read food labels: Pay attention to serving sizes and carbohydrate content.
- Listen to your body: Be mindful of how different foods affect your blood sugar levels and adjust your meals accordingly.
Remember: This is just a sample meal plan, and it's important to work with a healthcare professional to create a personalized plan that meets your individual needs and preferences. With a bit of planning and creativity, you can enjoy a delicious and fulfilling diet while effectively managing your diabetes.
Supplements: A Helping Hand, Not a Magic Bullet
While a balanced diet and exercise form the cornerstone of diabetes management, certain supplements can lend a helping hand. Think of them as trusty sidekicks, supporting your body's efforts to regulate blood sugar and ward off complications. But remember, they're not a substitute for a healthy lifestyle or medication. Always consult your doctor before starting any new supplements, as they can interact with medications or have unintended effects. Some supplements that may be beneficial for people with diabetes include:
- Magnesium: This mineral plays a role in glucose metabolism and may help improve insulin sensitivity.
- Vitamin D: Research suggests a link between vitamin D deficiency and an increased risk of diabetes.
- Omega-3 fatty acids: These healthy fats may help reduce the risk of heart disease, a major concern for people with diabetes.
- Cinnamon: Some studies show that cinnamon may help improve insulin sensitivity and blood sugar levels.
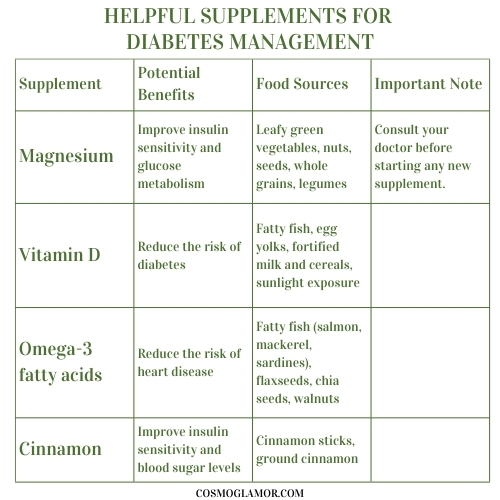
Remember, supplements are just that – supplements. They can complement a healthy lifestyle, but they can't replace it. Focus on the fundamentals first, and then discuss with your doctor whether any supplements might be a good addition to your diabetes management plan.
Conclusion: Embrace the Flavor, Embrace the Health
Navigating a diabetes diagnosis can feel overwhelming, but remember, you're not alone. Embracing a diabetes-friendly diet isn't about deprivation—it's about discovering a world of delicious and nourishing foods that fuel your body and spirit. By making mindful choices and prioritizing whole, unprocessed ingredients, you can take control of your health, manage your blood sugar levels, and savor the joy of eating.
Remember:
- This is a journey, not a race. Small, sustainable changes over time lead to lasting results. Be kind to yourself, celebrate your victories, and learn from any setbacks.
- Seek support. Connect with a registered dietitian or certified diabetes educator who can provide personalized guidance and support. They can help you create a meal plan that fits your lifestyle and empowers you to make informed choices.
- Don't give up on flavor. Experiment with herbs, spices, and healthy cooking techniques to create meals that are both nutritious and delicious. Remember, healthy eating should be enjoyable, not a chore.
Resources:
- Dietary patterns and prevention of type 2 diabetes: From research to clinical practice.
- Effects of dietary patterns on blood glucose control in patients with type 2 diabetes: A systematic review and meta-analysis of randomized controlled trials.
- The Mediterranean diet and type 2 diabetes prevention: A systematic review and meta-analysis
- Effects of low-carbohydrate diets on glycemic control in patients with type 2 diabetes: A systematic review and meta-analysis
- Plant-based diets and diabetes: A systematic review and meta-analysis
- The role of dietary fiber in the management of type 2 diabetes
- The impact of sugary drinks on the risk of type 2 diabetes: A systematic review and meta-analysis