Imagine this: you're diligently following your diabetes management plan, watching your carbs, staying active, and taking your medications as prescribed. Yet, you still feel a nagging fatigue, a subtle numbness in your fingers, and a persistent brain fog. Could something else be at play? Could a simple vitamin deficiency be undermining your efforts?

The truth is, if you have type 2 diabetes, you might be at a higher risk for vitamin B12 deficiency, a condition that can mimic or exacerbate some diabetes symptoms. This often-overlooked deficiency can have a significant impact on your energy levels, nerve health, and even cognitive function.
In this article, we'll delve deep into the connection between vitamin B12 deficiency and type 2 diabetes, exploring the causes, symptoms, diagnosis, and treatment options. We'll uncover why diabetics are more susceptible, how this deficiency can masquerade as other diabetes-related complications, and most importantly, how you can ensure you're getting enough of this vital nutrient.
The Vital Role of Vitamin B12

Vitamin B12, also known as cobalamin, is an essential nutrient that plays a crucial role in numerous bodily functions. Unlike some vitamins that our bodies can produce, we must obtain B12 through our diet or supplements.
Why is B12 so important?
- Nerve Health: B12 is vital for maintaining the health of your nervous system, ensuring proper nerve signal transmission and preventing nerve damage.
- Brain Function: This vitamin is crucial for cognitive function, memory, and mental clarity.
- Red Blood Cell Production: B12 is essential for the production of healthy red blood cells, which carry oxygen throughout your body.
- DNA Synthesis: It plays a critical role in DNA synthesis and repair, essential for cell growth and function.
The B12-Diabetes Connection
While the recommended daily intake of vitamin B12 is relatively small (2.4 micrograms [mcg]), a significant number of people with type 2 diabetes struggle to maintain adequate levels. A study published in the Journal of the American Board of Family Medicine found that up to 22% of individuals with type 2 diabetes may be deficient in B12, a rate significantly higher than the general population. But why?
Metformin: A Double-Edged Sword
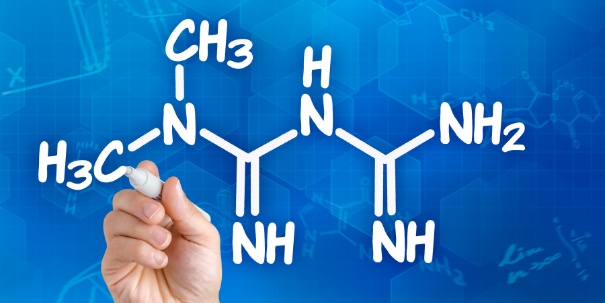
Metformin, a commonly prescribed medication for type 2 diabetes, is often the culprit. While highly effective in managing blood sugar levels, metformin can interfere with the absorption of vitamin B12 in the gut. This interference can lead to a gradual depletion of B12 stores over time, increasing the risk of deficiency. Research suggests that this interference may occur due to metformin's impact on calcium-dependent ileal transport, a key mechanism in B12 absorption.
The Intrinsic Factor Puzzle
Even if you're consuming B12-rich foods, your body might not be effectively absorbing it. B12 absorption is a complex process that relies on a protein called intrinsic factor, produced by specialized cells in the stomach lining. Intrinsic factor binds to B12 in the stomach, forming a complex that is then absorbed in the small intestine.
Several factors can impair intrinsic factor production or function, including:
- Pernicious Anemia: This autoimmune condition attacks the stomach cells that produce intrinsic factor, leading to significantly reduced B12 absorption.
- Age-Related Changes: While aging itself doesn't necessarily cause B12 deficiency, it can contribute to reduced stomach acid production, which is essential for B12 release from food and subsequent binding to intrinsic factor.
- Gastrointestinal Conditions: Conditions like Crohn's disease, celiac disease, and atrophic gastritis can damage the stomach lining and affect intrinsic factor production.
- Gastric Surgery: Procedures that remove or bypass parts of the stomach can also impact intrinsic factor secretion.
A Vicious Cycle: B12 and Blood Sugar
Interestingly, B12 deficiency itself can contribute to elevated blood sugar levels, creating a potential vicious cycle. While the exact mechanisms are still being investigated, it's believed that B12 deficiency may impair insulin signaling pathways, leading to reduced insulin sensitivity and increased blood glucose. This complex interplay between B12 deficiency and diabetes highlights the importance of early detection and intervention.
Recognizing the Signs

Vitamin B12 deficiency can be sneaky, with symptoms often mimicking other health issues or even going unnoticed in the early stages.
Early Warning Signs:
- Unexplained Fatigue: Feeling constantly tired even after adequate rest.
- Weakness: A general sense of weakness and lack of energy.
- Unintentional Weight Loss: Losing weight without trying.
- Loss of Appetite: Decreased interest in food.
- Constipation: Difficulty with bowel movements.
Long-Term Consequences:
If left untreated, B12 deficiency can lead to more serious complications, including:
- Permanent Nerve Damage: Leading to numbness, tingling, and pain, especially in the hands and feet (peripheral neuropathy – a condition affecting the nerves in the extremities).
- Cognitive Decline: Memory problems, difficulty concentrating, and even dementia.
- Mental Health Issues: Depression and mood changes.
- Impaired Mobility: Difficulty with balance and coordination.
The Neuropathy Puzzle
Diabetic neuropathy, a common complication of diabetes, can also cause numbness and tingling in the extremities. This overlap in symptoms can make it challenging to determine whether B12 deficiency is contributing to or even causing these sensations.
Diagnosing the Deficiency

If you suspect you might be deficient in vitamin B12, it's crucial to consult your doctor. A simple blood test can accurately measure your B12 levels and determine if supplementation is necessary.
Interpreting the Results:
- <200 picograms per milliliter (pg/mL): Generally considered deficient.
- >400 pg/mL: Sufficient levels.
- 200-400 pg/mL: May warrant supplementation, especially if experiencing symptoms.
Replenishing Your B12 Stores

Once diagnosed, replenishing your B12 levels is usually straightforward. Your doctor will recommend the appropriate treatment based on the severity of your deficiency and individual needs.
Supplementation Options:
- Oral Supplements: Readily available over-the-counter in various forms, including tablets and capsules.
- Sublingual Supplements: Dissolved under the tongue for faster absorption.
- B12 Injections: Often used for severe deficiencies or when absorption is impaired. These injections provide a mega-dose of B12 (typically 1 milligram [mg]) that can effectively replenish your stores.
Important Note: While B12 supplementation is generally safe, it's essential to consult your healthcare provider before starting any new supplement. In rare cases, high doses of B12 can cause side effects like acne, swelling, or rapid heart rate.
Dietary Sources:
While supplementation is often necessary to correct a deficiency, incorporating B12-rich foods into your diet is essential for long-term maintenance.
Top Sources of B12:
- Liver
- Clams
- Caviar
- Fish (mackerel, herring, salmon, tuna, cod, trout)
- Crab
- Organ meats (kidney, heart, giblets, brains)
- Eggs
- All meats and poultry
If you're a vegetarian or vegan, it's crucial to include B12-fortified foods or supplements in your diet, as plant-based sources are limited.
Are You At Risk?

While anyone can develop a vitamin B12 deficiency, certain factors increase your risk, especially if you have type 2 diabetes.
Risk Factors:
- Metformin Use: As discussed, metformin can significantly interfere with B12 absorption.
- Age: Our ability to absorb B12 can decline with age due to factors like reduced stomach acid production.
- Vegetarian or Vegan Diet: Animal products are the primary source of B12, making vegetarians and vegans more susceptible to deficiency.
- Gastrointestinal Issues: Conditions like celiac disease or Crohn's disease can affect nutrient absorption, including B12.
- Bariatric Surgery: Surgical procedures that alter the digestive system can impair B12 absorption.
- Family History of Pernicious Anemia: This autoimmune condition affects the production of intrinsic factor, essential for B12 absorption.
- Long-Term Use of Certain Medications: Besides metformin, medications like proton pump inhibitors (PPIs), H2 blockers, and some antibiotics can also interfere with B12 absorption.
If any of these risk factors apply to you, it's crucial to discuss B12 testing with your doctor. Early detection and treatment can prevent long-term complications and improve your overall well-being.
Beyond Supplementation: Lifestyle Strategies

While supplements are often necessary to correct a deficiency, lifestyle factors also play a role in optimizing your B12 levels.
Boosting Your B12 Naturally:
- Prioritize B12-Rich Foods: Include a variety of animal products in your diet, such as fish, poultry, eggs, and dairy.
- Optimize Gut Health: A healthy gut microbiome aids in nutrient absorption. Include probiotic-rich foods like yogurt and fermented vegetables in your diet.
- Manage Stress: Chronic stress can affect nutrient absorption. Practice stress-management techniques like meditation, yoga, or deep breathing exercises.
A Personal Perspective and Beyond
I remember when my own grandmother, a long-time type 2 diabetic, started experiencing unusual fatigue and tingling in her feet. She attributed it to her diabetes, but her doctor, thankfully, decided to check her B12 levels. Sure enough, she was deficient. After a few weeks of B12 injections, her energy levels soared, and the tingling subsided.
This experience isn't unique. Many individuals with diabetes may unknowingly suffer from B12 deficiency, mistaking its symptoms for other diabetes-related complications. A study published in Diabetes Care found that B12 deficiency was associated with an increased risk of peripheral neuropathy in type 2 diabetes patients, even after controlling for other factors like blood sugar control. These findings underscore the importance of considering B12 deficiency in diabetics experiencing neuropathy or other unexplained symptoms.
The Bottom Line
Vitamin B12 deficiency is a common yet often overlooked condition that can significantly impact the health and well-being of individuals with type 2 diabetes. The interplay between diabetes, metformin use, and B12 absorption creates a complex scenario that requires proactive awareness and management.
By understanding the signs and symptoms, recognizing your risk factors, and seeking appropriate testing and treatment, you can safeguard your B12 levels and prevent potential complications. Remember, optimal B12 status is not just about numbers on a lab test; it's about feeling energized, maintaining cognitive clarity, and protecting your nerve health for years to come.
Long-Term Monitoring and Prevention
Once you've corrected a B12 deficiency, it's crucial to maintain adequate levels over time. Your doctor may recommend periodic monitoring of your B12 levels, especially if you have ongoing risk factors.
For individuals with diabetes, routine screening for B12 deficiency can be a valuable preventative measure. Early detection and treatment can help avoid long-term complications and improve overall quality of life.
Cost and Accessibility
The cost of B12 testing and treatment can vary depending on your location and healthcare coverage. Oral B12 supplements are generally affordable and readily available over-the-counter. B12 injections may be more expensive and typically require a doctor's visit. If cost is a concern, discuss it with your healthcare provider to explore the most affordable options for you.
A Note for Everyone
While this article focuses on the link between B12 deficiency and type 2 diabetes, it's important to remember that B12 deficiency can affect anyone, regardless of their diabetes status. Individuals following a vegan diet, those with certain gastrointestinal disorders, or those taking medications that interfere with B12 absorption should be particularly mindful of their B12 intake.
If you have any concerns about your B12 levels or any of the information presented in this article, don't hesitate to discuss them with your healthcare provider.
Resources:
- Prevalence of vitamin B12 deficiency in patients with type 2 diabetes: a cross-sectional study.
- Association of biochemical B12 deficiency with metformin therapy and vitamin B12 supplements: the National Health and Nutrition Examination Survey, 1999-2006.
- Vitamin B12 deficiency in diabetic patients treated with metformin: A narrative review.
- Determinants of vitamin B12 deficiency in patients with type-2 diabetes mellitus — A primary-care retrospective cohort study.
- Association of vitamin B12 deficiency in people with type 2 diabetes on metformin and without metformin: a multicenter study, Karachi, Pakistan.