Diabetes is a complex condition that affects millions worldwide, and one of its lesser-known but crucial aspects is its impact on foot health. Due to nerve damage (neuropathy) and poor blood circulation (peripheral artery disease), people with diabetes are more susceptible to foot problems that can lead to serious complications. That's why prioritizing foot care is paramount for diabetics. This comprehensive guide will delve into the intricacies of diabetic foot care, empowering you with the knowledge and tools to maintain healthy feet and prevent potential issues.
Why is Foot Care So Important for Diabetics?

Diabetes can wreak havoc on your feet in ways you might not even realize. High blood sugar levels over time can damage the nerves, leading to a loss of feeling in your feet. This means you might not notice a cut, blister, or sore, allowing it to worsen significantly before you even know it's there.
Additionally, diabetes can impair blood flow to your extremities, making it harder for wounds to heal. This combination of nerve damage and poor circulation creates a perfect storm for infections and ulcers, which, in severe cases, can lead to amputation.
Think of it this way: Imagine your feet as a house.
- Neuropathy is like having a faulty alarm system that doesn't alert you to intruders (injuries).
- Poor circulation is like having weak walls that crumble easily (slow healing).
- High blood sugar is like a termite infestation, silently weakening the entire structure.
Without proper care, your “house” becomes vulnerable to serious damage.
But don't worry! By understanding the risks and taking proactive steps, you can significantly reduce the likelihood of complications and enjoy healthy, happy feet.
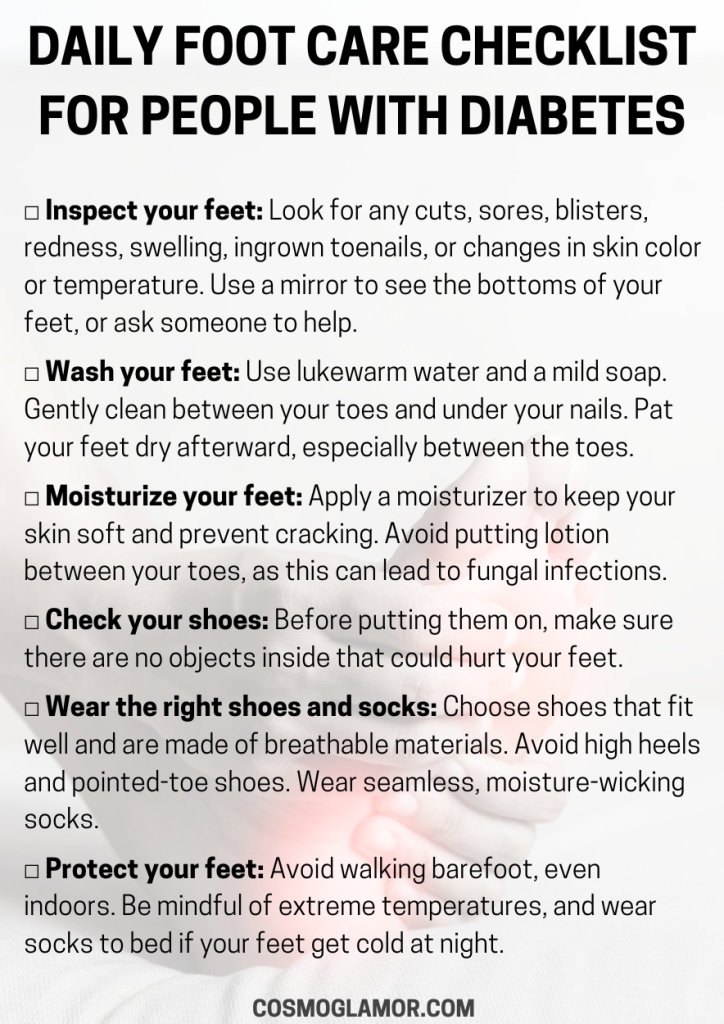
Daily Foot Care Routine

Think of your daily foot care routine as a series of checkpoints, ensuring everything is in order and addressing any minor issues before they escalate.
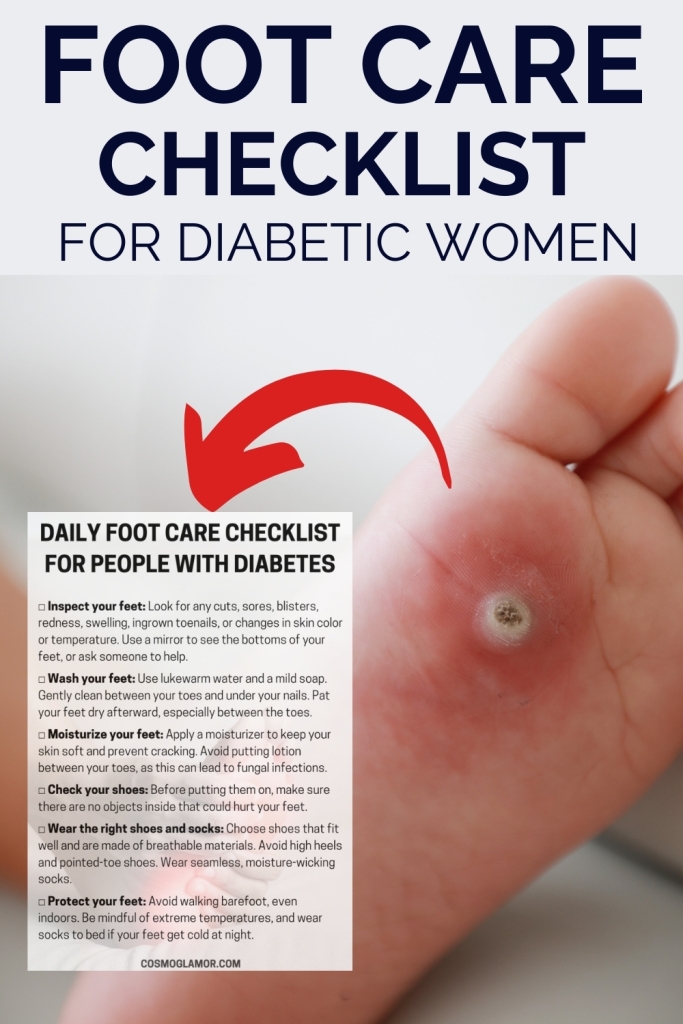
1. Inspection is Key
Every day, take a few moments to thoroughly examine your feet. Use a mirror to see the bottoms or ask a family member for assistance if needed. Look for:
- Cuts, sores, or blisters: Even the smallest nick can become a problem if left unnoticed.
- Redness or swelling: These could be signs of inflammation or infection.
- Ingrown toenails: These can be painful and easily become infected.
- Changes in skin color or temperature: These could indicate circulation problems.
Remember: Early detection is crucial. If you notice anything unusual, don't hesitate to contact your doctor or podiatrist.
2. Gentle Cleansing
- Wash your feet daily with lukewarm water and mild soap. Avoid soaking your feet, as this can dry out the skin.
- Water temperature matters: Always test the water temperature with your elbow before immersing your feet, as neuropathy can make it difficult to gauge the temperature accurately.
- Be thorough but gentle: Cleanse between your toes and under your nails, but avoid harsh scrubbing.
3. Moisturize with Care
- After washing, gently pat your feet dry, paying special attention to the areas between your toes.
- Apply a moisturizer to keep your skin soft and prevent cracking. However, avoid putting lotion between your toes, as this can create a moist environment that encourages fungal growth.
4. Nail Care Know-How
- Trim your toenails straight across and use a nail file to smooth any sharp edges. Avoid cutting your nails too short or digging into the corners, as this can lead to ingrown toenails. If you have difficulty trimming your nails or have any concerns, consult a podiatrist.
5. Footwear Matters
Wearing the right shoes and socks is crucial for diabetic foot health.
- Choose shoes that fit properly: Avoid shoes that are too tight or too loose. Make sure there is enough room for your toes to wiggle.
- Opt for breathable materials: Leather and canvas allow your feet to breathe, reducing the risk of moisture buildup.
- Say no to high heels and pointed toes: These styles can restrict blood flow and put excessive pressure on certain areas of your feet.
- Wear seamless socks: Seams can rub against your skin and cause irritation or blisters. Choose socks made of moisture-wicking materials to keep your feet dry.
- Break in new shoes gradually: Wear new shoes for short periods initially to avoid blisters and allow your feet to adjust.
6. Protect Your Feet
- Avoid walking barefoot: Even indoors, wear shoes or slippers to protect your feet from injuries.
- Check your shoes before putting them on: Make sure there are no pebbles, sharp objects, or other debris inside.
- Be mindful of temperature: Avoid exposing your feet to extreme heat or cold. Wear socks in bed if your feet get cold at night.
By incorporating these daily practices into your routine, you will be taking significant strides towards maintaining healthy feet and preventing complications.
Recognizing Potential Problems

Even with diligent daily care, problems can sometimes arise. Knowing what to look for empowers you to take action promptly.
1. Common Foot Problems in Diabetics
- Athlete's foot: This fungal infection causes itching, scaling, and redness, often between the toes.
- Fungal nail infections: These infections cause nails to become thick, discolored, and brittle.
- Calluses and corns: These thickened areas of skin can develop from pressure or friction.
- Dry skin: Diabetes can reduce sweat production, leading to dry, cracked skin.
- Foot ulcers: These open sores are a serious complication and require immediate medical attention.
- Charcot foot: This condition involves the breakdown of bones and joints in the foot, often accompanied by swelling, redness, and warmth.
2. When to Seek Medical Attention
Don't hesitate to contact your doctor or podiatrist if you notice any of the following:
- A sore or cut that doesn't heal within a few days
- Signs of infection, such as redness, swelling, warmth, pus, or red streaks
- Ingrown toenails
- Changes in skin color or temperature
- Numbness or tingling in your feet
- Pain in your feet or legs
- Any foot deformity or change in the shape of your foot
Early intervention is crucial in preventing serious complications.
Advanced Foot Care Strategies

Beyond the daily essentials, there are additional strategies and treatments that can help maintain optimal foot health.
1. Therapeutic Footwear
If you have certain foot conditions or deformities, your doctor may recommend therapeutic shoes or custom orthotics. These specialized footwear options provide support, cushioning, and pressure relief, helping to prevent ulcers and other complications.
-
Custom orthotics: These are inserts designed to fit your feet precisely and address specific foot problems like flat feet, high arches, or uneven pressure distribution. They can help correct foot imbalances, redistribute pressure, and reduce friction. Think of them as “prescription inserts” tailored to your unique needs, much like eyeglasses are for your vision. For example, someone with a bunion might benefit from an orthotic with a cutout that reduces pressure on the affected area.
-
Therapeutic shoes: These shoes are designed with extra depth, width, and cushioning to accommodate foot deformities and reduce pressure points. They often have seamless interiors and adjustable closures for a comfortable fit. They provide a protective and supportive environment for your feet, similar to how a cast protects a broken bone. For instance, someone with Charcot foot might need a therapeutic shoe with a rocker bottom to aid in walking and offload pressure from the affected area.
2. Regular Foot Exams
Seeing a podiatrist regularly is essential for people with diabetes. During a foot exam, the podiatrist will:
- Inspect your feet for any problems: They'll check for cuts, sores, blisters, calluses, and other abnormalities.
- Assess your circulation and nerve function: They may perform tests to check the blood flow and sensation in your feet.
- Provide guidance on proper foot care: They'll offer personalized advice on daily care, footwear, and other strategies to keep your feet healthy.
- Treat any existing foot problems: They can provide treatment for conditions like ingrown toenails, calluses, and ulcers.
The American Diabetes Association recommends a comprehensive foot exam at least once a year, or more frequently if you have existing foot problems.
3. Managing Underlying Conditions
Keeping your blood sugar levels under control is fundamental for preventing diabetic foot complications. Work closely with your healthcare team to manage your diabetes effectively.
- Medication adherence: Take your medications as prescribed and monitor your blood sugar regularly.
- Healthy lifestyle: Eat a balanced diet, exercise regularly, and maintain a healthy weight.
- Regular checkups: See your doctor for regular checkups and follow their recommendations for managing your diabetes.
By taking a proactive approach to your overall health and collaborating with your healthcare providers, you can significantly reduce your risk of developing foot problems.
The Power of Prevention
Remember, prevention is the most powerful tool in your foot care arsenal. By adopting a proactive approach and incorporating these strategies into your daily life, you can significantly reduce your risk of developing foot problems and enjoy healthy, active feet for years to come.
Think of foot care as an investment in your overall well-being. It's about more than just avoiding complications; it's about maintaining your independence, mobility, and quality of life.
Here's what Maria, a diabetic for over 20 years, shared about her experience:
“I used to take my feet for granted, but after a close call with a foot ulcer, I realized how important proper care is. Now, I follow a daily routine, wear the right shoes, and see my podiatrist regularly. It's given me peace of mind and allowed me to stay active.”
Take charge of your foot health today, and step confidently into the future!
Resources:
- The effectiveness of a multifaceted foot care program in reducing the incidence of diabetic foot ulcers
- Diabetic Peripheral Neuropathy: Epidemiology, Diagnosis, and Treatment
- The impact of diabetic foot complications on quality of life
- Therapeutic footwear for people with diabetes: A systematic review
- Effectiveness of foot self-care education programs for people with diabetes
- Risk factors for amputation in patients with diabetic foot ulcers
- Advances in the prevention and management of Charcot foot
- The role of telemedicine in diabetic foot care
- Economic burden of diabetic foot ulcers
- New technologies in diabetic foot care: A review of emerging trends